Post-Operative Rehabilitation
for Meniscus Surgery
Reasons for Undergoing Surgery
When dealing with a meniscus injury of the knee, there could be many reasons for a physician to recommend surgery. From a more general standpoint, the physician will try to take into account ALL factors (pain, quality of life, surgery risk, etc.) in determining whether surgery is of net benefit to you. In some cases, this is a simple determination if the patient is relatively young, in good health and the meniscus tear is located in an area where there is NO blood flow (the inner 1/3 of the meniscus is located outside of the vascular zone). In other cases, surgery is typically the final resort option when recommended conservative treatment options have failed to help.
 If you are undergoing surgery for a torn meniscus and the tear is in the vascular zone, it is most likely that you have undergone a course of conservative treatments for at least six weeks - as recommended by your doctor. They do this because it is generally understood by doctors and surgeons that meniscus surgery will introduce more scar tissue into the knee. This added scar tissue will be problematic, requiring more physical therapy and conservative treatment options post-surgery. If proper recovery protocols are not undertaken following the surgery, your knee joint could wind up in worse shape than it was before the surgery! This is why surgery is only performed as a last resort.
Most doctors, physicians and orthopedic specialists will recommend a course of conservative treatments for minor meniscus injuries before considering surgery.
Some conservative treatment methods recommended include:
- Rest - This is important for initial recovery; rest and elevation will help reduce pain, swelling and inflammation in the early stages of injury. This can be difficult when you have to carry on with daily activities, but resting and elevating your knee whenever you can is recommended. During your recovery you will probably have to modify or avoid the activities that put stress on your knee until your pain and inflammation settles. However, too much rest can also be harmful, as knee and ankle immobility can actually cause stiffening in the joints. This is why rest should be used when reducing initial pain and swelling, but should not be considered for more long-term conservative treatment.
 - Avoid Activities that Caused Your Knee Injury - While resting your injury it's also important to avoid all activities that may have caused your knee damage (especially any strenuous or repetitive movement). Continuing on with regular activities can increase the severity of your injury, turning a mild to moderate case of tissue damage into a downward spiral that can often severely impact your life. Also, trying to 'work around' your injury will eventually give rise to over-compensation injuries in other areas of your body.
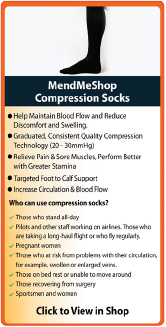
- Use a Cold Compress or Ice Pack - Cold is very effective at reducing pain and inflammation - use at the onset of the injury and during flareups.
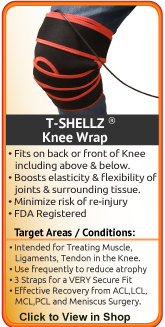
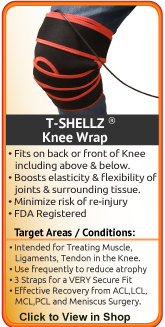
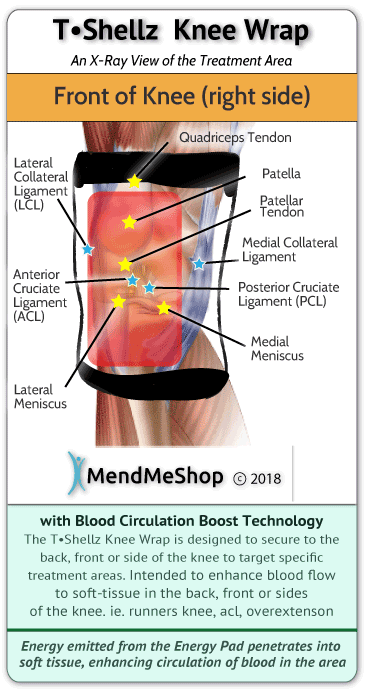
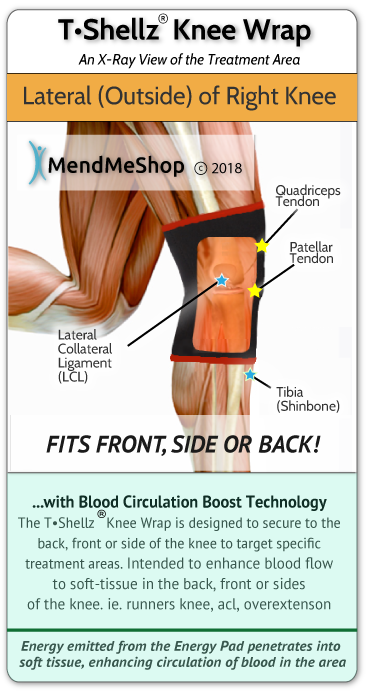
- Use a Knee TShellz Wrap® - Once swelling has been reduced, you can use your own blood flow to maximize your rehabilitation. Improved blood flow to your knee in most cases will help improve recovery time while improving overall health of soft tissue in the area. Knowing the body uses blood flow to heal soft tissue, this wrap is intended to maximize your rehabilitation by maintaining a healthy blood flow to soft tissue. Increased blood flow to damaged soft tissue should augment the bodys' own repair process, helping decrease recovery time while reducing re-injury risk. Promoting blood flow and heat to the treatment area will help to minimize the growth of scar tissue, increase tissue flexibility and help reduce onset of atrophy. This is why we recommend a TShellz Wrap treatment before undergoing activity - an increase in flexibility should help reduce risk of further injury while also assisting in the battle against atrophy. Heat via the TShellz Wrap® is especially helpful in dealing with chronic tendon & muscle injuries or on-going pain and stiffness from a strained knee.
- Use a Knee Support & Compression Sleeve - If you are experiencing discomfort or a feeling of knee instability, the MendMeShop Knee Sleeve is designed to help. The compression sleeve will move easily with your body with no stiffness in the sleeve itself despite being compression apparel. The sleeve is designed not to chafe the skin and reduce stiffness, swelling, and inflammation in the joint.
- For reducing discomfort while resting, (or to get some sleep) consider a High Quality Back Pillow and/or Knee Pillow for comfort while sleeping or sitting
- Try to Avoid Over Compensating for your Injury on your "'Healthy' (Non-Injured) Side - Many people will start limping or carrying objects with their opposite arm to compensate for their leg injury. Our bodies can adapt easily to any changes, including a hamstring injury. This quick adaptation could mean that you are already compensating for your injury without even knowing it!
When you compensate for your injury by using your opposite ('healthy') arm, leg, shoulder, knee, foot, etc. - then you are putting more weight and pressure on that side of your body. In many cases, your dominant side was injured (if you're right-handed this would be your right side) so your weaker side is trying to pick up the slack! The pain, stiffness, swelling and inflammation you then get on your 'healthy' side is something referred to as 'over-compensation pain'. Over-compensating for your injury can lead to other injuries and as such, it is important to be aware of how you are compensating so you can be extra careful; if there is an overcompensation flareup, treat this with the same conservative treatment methods to keep in under control.
- Rehabilitative Stretching under supervision of a PT or doctor. The intent of this is to provide you with increased range of motion, pain relief and strengthening of the surrounding tissue of the joint. Doctors or surgeons typically won't perform a surgery until they feel that their patient has put effort into treating their injury with conservative treatment methods. This may include up to 4 to 6 months of visits to a PT clinic. If you haven't experienced any improvement in your condition during that time then surgery may be considered. Agressive PT approaches may focus on forced or manual manipulation of the leg/knee - this means your physical therapists will be trying to move your knee past the point of comfort as they strive to increase range of motion and prevent further atrophy. This can be painful and end up making your injury worse if not done correctly. (reference: 1)
- Stretching - Stretching your joint in PT and at home will help you to regain your range of motion much faster than not stretching at all. Stretching in many ways is key maintaining good Range of Motion (ROM) in your joint, and stretching can be made much easier with use of a TShellz Wrap® before to warm up soft tissue, and a Cold Compress or Ice Pack treatment after to prevent any return of swelling and inflammation.
Injections
In most cases, your Doctor will start with non-surgical treatments options. Some of the options your doctor may recommend include anti-inflammatory medication to manage pain and inflammation. Steroid injections are advised with caution for any type of tendon condition as there is increased risk of tendon rupture.
(reference: American Academy of Orthopaedic Surgeons)
Restricted Movement Is Risky If It Goes On For Too Long
There are risks associated with regular use of a knee brace, especially if the brace you are using is not a custom fitted/design. If you are using a standard or "off the shelf" knee brace then it is possible that the brace is not the right size, positioned incorrectly on your knee, or even causing more damage to your injury. Knee braces can also feel heavy or bulky at first if you are not used to wearing one. It is possible that you may not feel the benefits of wearing a knee brace for a month, or however long it takes for you to feel comfortable wearing your brace. Skin irritation can also occur under the brace depending on the breath-ability of the material you are using for your knee brace and the overall fit. One important thing to be aware of is the amount of restriction you are placing on your knee while wearing a knee brace. Too much restriction in movement for an extended period of time can result in stiffness of your joint, chronic pain, or wasting away of the ligaments, tendons and muscles in your knee and leg.
Safe, Effective Conservative Treatment Options are Available
If you are not at the surgery stage and your physician has opted to recommend conservative treatment options, we recommend you talk with your physician about including the TShellz Wrap® in your conservative treatment protocol. If surgical intervention is required, talk with your physician about using these same products for post-surgery recovery as you will find them to be highly effective for reducing post-surgery inflammation, enhancing range of motion and minimizing scar tissue growth.
If Surgery is Required...
Most doctors, physicians and orthopedic specialists will recommend conservative therapy for minor meniscus injuries before considering surgery. If all conservative treatment methods have been explored and your symptoms (reduced range of motion, clicking, locking, pain) persist, then you will be considered a candidate for surgery. You and your doctor may decide to move forward and have you undergo surgery, which will trigger the next chapter of your recovery journey. Your post surgery rehabilitation efforts will have an important impact on how soon you can return to living and enjoying your normal daily life.
If possible, avoiding surgery is typically the best option. However in some some cases meniscal repair or even a meniscectomy is advised. Surgical removal of a meniscus (a procedure called a meniscectomy) may be necessary if the meniscus is worn down too much and/or is damaged beyond repair. Artificial meniscal implants might be used following a meniscectomy but the success rate of meniscal implants is currently found to be low (reference: boneandjoint.org.uk).
If you need to have meniscal surgery, we highly recommend you incorporate AidMyMeniscus's conservative treatment options during your post-surgery recovery. Using proper conservative treatment protocols when recovering from surgery can be extremely beneficial for:
- Reducing post-surgery inflammation with a Cold Compress or Ice Pack.
- Enhancing range of motion (elongation) and elasticity of your soft tissue by introducing heat via the Knee TShellz Wrap®.
- Enhancing blood circulation (the body's organic healing process) by introducing the use of a Knee TShellz Wrap®.
Important: Do not start TShellz Wrap® treatments until the surgical skin wound has healed over and inflammation has reduced in the area (generally 2 to 6 weeks after surgery)
The type of surgery you will have depends on the type of meniscus injury you are faced with.
If you have undergone surgery on your meniscus then your physician will quickly get you on the path to rehabilitation. Now, the aggressiveness of the rehabilitation efforts will depend on a variety of factors including (but not limited to): your age, the state of your injury before surgery, the location of the meniscus tear (is enough blood supply available?) and how soon will you return to normal activity.
Usually, for quicker rehabilitation a partial meniscectomy will be performed. For meniscal repair surgery, however, the rehabilitation efforts can vary widely. It's important to be aware of the risks you may face with any procedure intended to fix or relieve pain from your meniscus injury.
It is quite common to have a tendon or ligament injury at the same time as meniscus damage.
When it comes to meniscus surgery there are common procedures that are used to treat your meniscus tear. The most common forms of meniscus surgery are generalized as follows:
- Open Knee Surgery
- Arthroscopic Meniscal Repair Surgery
- Arthroscopic Partial Meniscectomy Surgery
- Arthroscopic Meniscal Replacement Surgery
Meniscus surgery is typically done arthroscopically while the patient is under some type of anesthesia. Arthroscopic surgery usually does not require an overnight hospital stay though this is not always the case. Your orthopedic surgeon will determine which surgery is most suited to your condition. There are rare cases where your surgeon may change to open surgery during an arthroscopic procedure to correctly repair all the damage to the tissue in the knee.
Click here to read more about specific types of meniscus surgery
Meniscus Zones: Red Zone versus White Zone
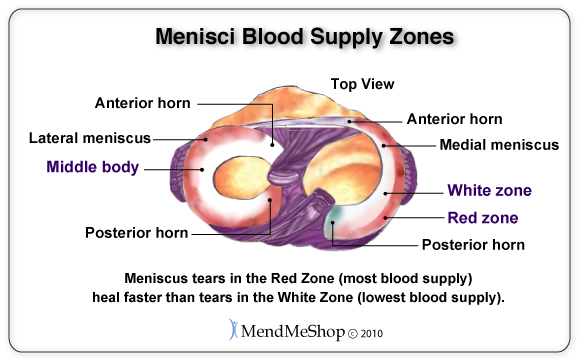
Doctors call the outer third area of the meniscus the Red Zone. This is the area of the meniscus that receives the most blood flow. The inner two-thirds area of the meniscus is deemed the White Zone and this is the area of the meniscus that receives very little blood flow. If you have read through this website, you will know that blood flow is essential for healing - as such, the White Zone of the meniscus is troublesome as this area does not heal very well.
Meniscus Surgery Recovery
If you have undergone surgery on your meniscus injury then your physician will quickly get you on the path to post-surgical rehabilitation. Now, the aggressiveness of your rehabilitation efforts and your injuries ability to heal will depend on a variety of factors including (but not limited to):
- your age, overall health and activity level
- the state of your injury before surgery (severe injuries like a tendon rupture, open wound, bone damage or fracture will require more intense surgery)
- the type of surgery you have undergone
- how soon you must return to normal activity
It is also important to keep in mind that no two meniscus injuries and surgical procedures are alike. So if you and a friend suffer from meniscus injuries at the same time, your rehabilitation after meniscus surgery is going to be completely different from that of your friend's. This is why rehabilitation plans need to be tailored to your personal needs. If you are consulting a physical therapist rather than your surgeon for rehabilitation, your physical therapist will need an account of your injury before the surgery and what was done during your surgery before properly creating a rehabilitation plan suited to your specific needs.
Rehabilitation and physical therapy efforts after a meniscal repair differ with two distinct schools of thought between orthopedic surgeons, doctors, and physical therapists. Some medical professionals will recommend a conservative method of rehabilitation, while others will offer accelerated guidelines for physical therapy.
For conservative treatment methods, patients are required to use rest, cold compression, and limit mobility and weight bearing on the affected knee until 4 weeks after the surgery. Range of Motion (ROM) exercises are also limited until 6 weeks after surgery, and a full return to a normal level of activity or sports training is not encouraged until 5 to 6 months after the surgery.
On the other hand, accelerated rehabilitation encourages early ROM stretching and weight bearing exercises. An accelerated rehab program provides no limits for getting back to activity though this is more or less evaluated on a case by case basis.
There have been many studies comparing and contrasting the two techniques to find which is more effective and better for the body, however results in these studies vary - resulting in no clear advantage of one technique over the other. The approach for rehabilitation after a meniscal repair is treated much like the orthopedic surgeon's decision for which surgical procedure will be selected - rehabilitation hinges on the age of the patient, condition of the meniscus pre and post surgery, and of course the dedication of the patient to the rehabilitation program.
Your rehabilitation will be based on the type of surgery you have had. Recovery from meniscal repair surgery will usually take longer to heal and require more restriction of movement than the rehabilitation from a partial meniscectomy procedure. Rehabilitation after open knee surgery is always more extensive than rehabilitation after an arthroscopic procedure, because open surgeries are more invasive. It is important to note that driving after a meniscal repair is usually not recommended by a doctor until you have full control of your knee back and do not need to take prescribed medication to manage your pain. You will typically have to wait 4 to 6 weeks after your meniscal repair to return to driving. This timeline will of course depend on whether your doctor has selected a conservative or aggressive plan for your rehabilitation.
Meniscus Surgery Rehab - What You Can Generally Expect
Initially following a meniscal repair, the knee is usually immobilized in full extension with a postoperative immobilizer which is eventually replaced with a long leg brace. This brace is worn continuously (expect during rehabilitation exercises) for at least 2 weeks, with the range allowance of the brace increasing as the weeks progress. This continues until the knee can be fully flexed. Note, in some cases such as a central zone repair or a meniscal transplant the brace may be necessary for 6 weeks or longer. Following a partial meniscectomy, immobilization is not required and full extension with 90 degree flexion is possible approximately 10 days after surgery.
With a meniscus repair you may be allowed to bear some weight on your repaired knee with the assistance of crutches and a brace immediately following surgery. The amount of weight and progression of weight allowed will depend on your specific case. However, you will be able to bear full weight within 4-8 weeks if your quadriceps muscle control is good. In the case of a partial meniscectomy, you should be able to bear full weight within 4-7 days.
The goal of professionally led exercises during the first month of rehabilitation is to regain range of motion in the joint, regain muscle control in the leg, ensure the patella does not lose mobility, maintain flexibility and strength in the hip and ankle, and restore stability. Your doctor, surgeon or physical therapist will assist you with these exercises to achieve these goals without causing re-injury.
Following a meniscal repair, typical recommendations are to avoid pivoting, squatting, twisting and deep lunging exercises for at least 4-6 months following surgery. Jogging or running should be avoided for 5-6 months of rehabilitation. Generally you will be able to return to normal activities and sports approximately 6 weeks after a partial meniscectomy and 3-4 months after a meniscal repair or replacement. However, it is always recommended that you get your surgeons approval before beginning any exercises or activities following meniscus surgery.
Research indicates pain relief after a partial meniscectomy or abrasion is about 50 - 75%. Healing and recovery time is generally dependent on the degree of damage done, your age, pre-injury level of function, and your rehabilitation. Tenderness, pain, stiffness and weakness are very common after surgery.
A list of quick links to the types of surgery and post recovery:
Open Knee Meniscus Repair Rehabilitation
An open meniscus repair surgery is rarely performed because arthroscopic surgical techniques are much less invasive with a quicker rate of recovery and a better outlook for overall healing. If you have had an open knee surgery repair for your meniscus repair, you probably suffered from an acute trauma with an open wound over your knee, or your surgeon started an arthroscopic knee procedure but your injury was worse than he/she had predicted. This change of plans for your surgery is rare and never foreseen.
You should expect your rehabilitation to be longer if you have had open knee surgery. You will not know the full extent of your rehabilitation unless your surgeon has given you a detailed rehabilitation plan after the surgery. It is entirely possible that you will go into your surgery expecting the rehabilitation time period of an arthroscopic procedure, and come out of your surgery having to follow a longer rehabilitation period for open surgery. Orthopedic specialists do their best to diagnose your injury and plan for every stage of your surgery, but sometimes changes in their procedures are unavoidable.
What is known is that open knee surgery recovery can be similar to the recovery from a complete or partial knee replacement. Both procedures are invasive, require an incision 6 to 10 inches in length. You will have to stay in the hospital for a few days after your knee surgery, as you will be considered an inpatient for surgery.
Phase 1: In-Hospital Recovery
Timeline: End of Surgery to 4 days after Surgery
While in the hospital, your knee will be checked on periodically to see your how your are healing. The dressing on the 6 to 10 inch incision will be changed, and any excess fluid (blood) will be drained from the dressing. You may be encouraged to move your foot and lower leg to increase localized blood flow and manage all swelling and inflammation in your knee. Your doctor and/or surgeon will also monitor the swelling and any evidence of blood clot formation as these are some of the major side effects experienced after extensive surgery of this kind.
During your hospital stay you may interact with a physical therapist to introduce simple knee exercising meant to prevent atrophy (wasting away) of your muscles while you are resting your leg.
Phase 2: Initial At-Home Recovery
Timeline: 5 days to 8 weeks after Surgery
You will need to use crutches for approximately 4 weeks to reduce the amount of weight you are bearing on your affected knee/leg. This will help to protect the delicate work that has been done to fix the meniscal (and other) tissues in your knee as well as the outside skin incision(s). Your surgeon will recommend that you manage all post-surgical swelling using the R.I.C.E. formula (rest, ice, compression, elevation), as needed in the beginning, and then later whenever pain and swelling are experienced.
Your leg/knee will be stiff and painful at first, and simple, easy movements may seem challenging in the beginning. Don't be discouraged! Your overall mobility will be much more reduced than you anticipate because of the 6 to 10 inch incision on your knee. Some of this pain and stiffness can be treated by increasing healthy blood flow to your knee before you exercise, with a Knee TShellz Wrap®. The TShellz Wrap® will warm your tissue, reduce lingering stiffness in the knee, and increase the amount of oxygen, nutrients and water (basically energy) that travel to your injured tissue. Physical therapy will progress with regular appointments (1 to 2 times per week) for the first 8 weeks after the surgery. Exercise and strengthening routines will be focused on regaining simply abilities, such as walking, and improving the strength, capability and ROM of your knee.
Using a Knee TShellz Wrap® for approximately 15 to 20 minutes (finishing 15 minutes before exercise or your physical therapy appointment) will warm up your knee, relax your thigh (quadricep) muscles and boost flexibility of your tissue. Your commitment to recovery will include your physical therapist requesting you to continue your stretching at home to increase your rate of recovery.
You may be able to return to driving approximately 4 to 8 weeks after the surgery. At the same time, you may also be able to return to other low-impact daily activities, such as walking or cleaning the house.
Phase 3, Gradual Return to Regular Use and Activity
Timeline: 2 months to 1 year after Surgery
Physical therapy should continue for another few months (usually to at least 6 months) after the surgery with a gradual return to activity. High-impact activities, such as jogging or sports of any kind, may not be appropriate for at least a year after your surgery. Your overall ability to return to your normal set of activities will be judged on an individual basis with your surgeon and/or physical therapist. After rehabilitation has ended, you will need to continue the management of your knee healing through regular exercise and conservative treatments. Back to the surgery list
What's Overcompensation Pain?
Everything in the human body is connected. Any meniscus injury can lead to other injuries over time if not treated properly. You might start limping on the leg of your injured knee and place more weight on your opposite, healthy leg. Limping your way around for a long period of time may lead to pain in the knee, hip or lower back on your injured side because you are mis-aligning your entire leg (keeping it straight and off to the side) to compensate for the injury.
Rehabilitation after an Arthroscopic Meniscal Repair Surgery
As mentioned before, there are two different approaches to meniscus surgery recovery - a conservative plan and and aggressive plan. We have provided both rehabilitation methods but it is up to you to discuss the pros and cons of each approach with your doctor, surgeon or physical therapist to find out which rehabilitation plan will work best to heal your meniscus.
Conservative Rehabilitation for Meniscal Repair
Phase 1, Initial Recovery after Surgery
Timeline: Completion of Surgery to 6 weeks after Surgery
The main goals during this stage are to protect the meniscus repair, control pain and swelling, and encourage maximum healing potential. Right after surgery your knee will be wrapped with a bandage to protect the small key-hole incisions made in the skin. During the first few days of recovery you will need to change your bandage regularly to prevent infection. You will be strongly advised to not get your knee wet in any way within the first 2 days after your surgery.
You will be required to use crutches when walking to reduce the amount of weight you are bearing on your affected knee. You may gradually reduce use of your crutches throughout Phase 1 of your rehabilitation. You will also need to wear a locked knee brace (fitted before your surgery) for all weight bearing activities and while sleeping. The use of crutches and a locked knee brace will provide maximum protection for your knee while your meniscus goes through its' natural healing process.
It is important during this time to regularly control your pain and inflammation with a cold compression. Some doctors will refer to this cooling therapy as R.I.C.E. Applying cold to your knee will reduce pain by gently numbing the nerve-endings in your knee, and also slow down the inflammatory process effectively reducing swelling. While doing this, the cold helps stop continued tissue break-down, minimizing further soft tissue damage (this is very important after surgery).
Your doctor may suggest some light initial stretching to gradually introduce activity back into your routine. Light stretching may include active-assisted range of motion exercises like extending your knee, flexing your knee, raising your leg (quadriceps sets) or sliding your heel away from your body (heel slide). Your commitment to recovery will include stretching at home to increase your rate of recovery. Any exercises undertaken during rehabilitation must be cleared with your surgeon and physical therapist. If your surgeon has recommended the use of a physical therapist, you can expect to have regular weekly appointments scheduled during this phase.
You will also likely have a follow-up appointment with your surgeon to assess the progress your meniscus has made in healing after the surgery. If progress has been made and you are already undergoing light stretches, this is a good time to chat with your surgeon/physician about introducing heat therapy treatment via the use of a Knee TShellz Wrap®. Enhanced blood flow, introduced via the TShellz Wrap® will help maximize the body's natural repair process while temporarily increasing length and flexibility of soft tissue for minimization of re-injury risk while helping prevent range of motion loss.
Your doctor will advance you to the next Phase of rehabilitation when you can walk pain free without the aid of crutches and there is no evidence of inflammation or swelling in your knee.
Phase 2, Increase ROM and Weight Bearing Activity
Timeline: 6 weeks to 3 months after Surgery
Conservative rehabilitation will focus on gaining back your range of motion (ROM) and increasing your ability to bear weight on your leg. You may still be expected to wear a hinged knee brace, but it will no longer be locked.
You will start gradually moving your knee in a free (non-forced) way with very low-impact exercises such as: flexing of your knee, stationary bicycling, and strengthening of your leg muscles (quadriceps, hamstrings, thighs and calves). Many of these exercises will be geared to improving balance and strength within your hips and core. You will find over time that these stretches and exercises with build Range of Motion (ROM) in the knee, while increasing strength in the muscles surrounding the knee. Overall, this will help to increase the stability of your entire leg while healing.
You can expect to continue your regular physical therapy appointments approximately once every 1 to 2 weeks. It will be important that you completely dedicate yourself to your rehabilitation by stretching and exercising at home as well. Your physical therapist or doctor may give you specific guidelines for performing or adapting your physical therapy exercises at home.
Controlling post-exercise swelling and inflammation is crucial during this Phase. Any sign of swelling or inflammation after exercise is a sign of minor re-injury to your knee or surrounding muscles. Controlling your inflammation immediately after exercise for at least 15 minutes with a Cold Compress or Ice Pack will help reduce chance of re-injury to your meniscus. A set-back at this point could result in additional tearing of your meniscus.
Once you are doing exercises/stretches regularly and the inflammation is down, we recommend the use of a Knee TShellz Wrap® BEFORE exercise, workouts or activity of any kind to increase elasticity of knee joint ligaments & tendons and decrease chance of re-injury.
Your doctor will advance you to the next Phase of conservative rehabilitation once you are able to walk normally, show measured improvement with your ROM and demonstrate improved function and balance on your knee.
Phase 3: Optimize Full Capability of Your Knee
Timeline: 3 months to 6 months after Surgery
Your physical therapist or doctor may increase the number of repetitions that you must do for each stretch, and they may also introduce resistance or weights to the knee exercises. The goal of this Phase is to imitate movement and demands required of your body on a normal daily basis. This goal will be different for everyone. If for example you are an athlete, your physical therapist will likely introduce activity or drills that re-condition your knee for the sport that you're involved in. If you are not an athlete, your exercises will be more geared toward your personal level of activity based on any job-related or lifestyle demands that are placed on your body.
You will still need to keep your regular physical therapy appointments 1 to 2 times per week. You must also continue to control any post-exercise swelling and inflammation. Eventually, as your knee heals, you will experience decreased amounts of post-exercise swelling. Even if you do not immediately feel or notice any amount of inflammation after activity, you should still apply cold compression to eliminate any risk of recurring inflammation. Eliminating your inflammation encourages your body to heal quickly and efficiently.
Your doctor will advance you to the next Phase of rehabilitation once you are capable of full ROM and control of your knee without evidence of pain or swelling.
Phase 4, Return to Regular Use & Activity
Timeline: 6 months after Surgery and Beyond
After 6 months of successfully conservative rehabilitation your doctor will clear you for a full return to athletic and work activities. At this point you may have less involvement from your doctor or physical therapist. They may recommend occasional check-ups or appointments to assess your injury, but the responsibility of monitoring your progress will likely fall on your shoulders. After your rehabilitation has ended, you will need to keep a watchful eye on activity performed with your knee and address any signs of re-injury as soon as they occur. Back to the surgery list
When to use a TShellz Wrap (HEAT):
- AFTER the skin wound has fully healed.
- AFTER bruising has significantly reduced.
- NOT WHEN THERE IS SIGNIFICANT SWELLING.
- BEFORE getting out of bed in the morning.
- BEFORE going to bed at night. Never sleep during a treatment.
- BEFORE exercise, workouts or activity of any kind to increase elasticity of joint ligaments & tendons and decrease chance of re-injury.
- Anytime you feel your knee may have stiffened up, is tight and your mobility is reduced causing you more pain.
- Anytime BEFORE you feel you might undertake activity that will put significant strain on the injury area.
- Any other situation where you need to increase blood flow to your knee to relax the joint, relieve trigger point pain / spasms, prevent re-injury and enhance flexibility of soft tissue.
Accelerated (Aggressive) Rehabilitation for Meniscal Repair
Phase 1: Initial Recovery after Surgery
Timeline: Completion of Surgery to 1 week after Surgery
This phase is focused on protecting your knee after surgery and controlling pain/swelling while starting gentle movement of the knee and strengthening your quadriceps muscle. Your knee will be bandaged and you will need to change your bandage regularly to prevent infection at the site of your incisions. You may be fitted for crutches before the surgery, and will be expected to use these along with a locked knee brace for the first week after your surgery.
You will be encouraged to bear as much weight as you can handle on your knee while walking with the crutches. Controlling pain and inflammation with a Cold Compress or Ice Pack is important to stimulate healing of your meniscus and allow you to control inflammation - your doctor may refer to this as R.I.C.E. Using cold therapy will be important throughout the accelerated rehabilitation plan, because you will need to be sure to control any inflammation that occurs due to your exercising, stretching and strengthening routines. Inflammation could be a sign of re-injury to your meniscus - this is why cold compression will be important especially when it is applied after activity of any kind (exercising or extra walking around). You should apply cold for 15 to 20 minutes at a time as needed to reduce pain and inflammation.
Your doctor will start you off with gentle stretching of your quadriceps muscle. Some other exercises that your doctor may recommend include: extending of your knee by propping your heel up on furniture (heel prop), sliding your heel away from your body while in a seated position (heel slide), or flexing your ankle to stimulate circulation in your leg (ankle pump).
There may be some overlap between the 1st and 2nd Phases of accelerated rehabilitation. Your doctor or surgeon will likely schedule a post-operative check-up within 10 to 14 days after your surgery. For some, this will extend your 1st Phase of rehabilitation, for others your doctor may have already given you specific instructions about moving forward through your rehabilitation. Either way, your doctor will assess the healing progress of your meniscus at your appointment and discuss your rehabilitation plan so far.
Phase 2: Increase ROM and Weight Bearing
Timeline: 1 week to 5 weeks after Surgery
You will begin to focus on regaining your ROM and begin more in muscle strengthening. Controlling inflammation and swelling is still a key in this Phase, as increased motion without proper use of cooling therapy may put your meniscus at risk for re-injury.
You will be encouraged to continue using crutches when walking, and your knee brace will probably remain in a locked position. As with Phase 1, you will be able to bear as much weight as you can tolerate on your affected leg as long as you are using the crutches and knee brace as directed. The crutches will continue to help you distribute weight away from your affected leg, so you can continue to protect your meniscal repair throughout rehabilitation.
At this point if your doctor or surgeon feels a physical therapist will be a good time for your rehabilitation, you will likely have regular appointments 1 to 2 times per week. Your exercise plan will include stretches mentioned in Phase 1 along with new stretches focused on tightening the muscles in your leg and increasing range of motion. This may also include more involved quadriceps stretching, increased extension of the knee, gentle squats or other equipment, and maybe even a stationary bicycle if your ROM has improved to a satisfactory level. Any hamstring stretches, deep squats or activity that requires twisting of your knee should be avoided. Your doctor or physical therapist will also encourage you to continue the set of approved stretches at home as directed. Consistent movement both in your appointments and at home is crucial for the accelerated rehabilitation plan.
Once stretching is introduced, if swelling is down and the surgery skin wound has healed, talk to your physician about incorporating Circulation Boost via a Knee TShellz Wrap®. When used for approximately 10 to 15 minutes (finishing 15 minutes before exercise or your physical therapy appointment), heat from the wrap will help warm up soft tissue in the knee, relax your thigh (quadricep) muscles and boost flexibility of your tissue while reducing risk of re-injury to the delicate repair done on the meniscus. This boost of blood to the tissue will increase your natural healing and take full advantage of all the energy and hard work you are putting into your exercises.
You will advance to the next Phase of accelerated rehabilitation once your doctor of physical therapist feels you have marked improvement in your ROM.
Phase 3: Optimize the Full Capability of Your Knee
Timeline: 5 weeks to 10 weeks after Surgery
Your doctor or physical therapist will increase your activity level in order to regain full ROM and muscle strength in your leg. You may be able to stop using your crutches at this point if your doctor feels you have healed enough to bear more weight on your leg. It is important, if you are not going to be using the crutches any longer that you focus on walking slowly and normally. Limping should be avoided at all costs, as abnormal walking could result in re-injury of your meniscus or injury to your opposite leg, feet, hip or even your back with overcompensation injury/pain. You should also avoid squatting or pivoting on your injured knee.
Continued use of R.I.C.E. will be recommended, especially after activity, in order to control pain and inflammation. This therapy may be recommended 2 to 3 times per day for 15 to 20 minutes at a time.
Your exercise will be increased to include regular use of a stationary bicycle, or you may even be introduced to a pool program which will require running and exercising in the pool. Using a pool for rehabilitation is common, as the pool will shift your weight effectively reducing the amount of weight you are bearing on your affected knee during more complex movement. Stretching will continue to include stretches mentioned in both Phase 1 and 2 of this rehabilitation plan, but may also expand to include lunges, hamstring curls, and movement of your hip. The number of your stretches will have increased since Phase 1, and will continue to increase in order to regain full ROM and strength in your leg.
You will advance to the next Phase of rehabilitation once your doctor or physical therapist feels you have regained full ROM without pain in your knee. You must also have no pain or tenderness in your knee and may need to pass a clinical exam or a test of your muscular strength.
Phase 4, Return to Regular Use & Activity
Timeline: 10 weeks after surgery and beyond
At this phase, your doctor or physical therapist will most likely clear you for a return to work or athletic activity. It will be recommended that you continue your muscle strengthening and stretching in order to maintain healthy ROM of your knee. Pivoting and twisting on your knee should still be avoided when possible as your meniscus is still healing. Additional cardiovascular exercise will also be encouraged such as 20 to 30 minutes on a treadmill, stationary bicycle, elliptical trainer, or swimming approximately 5 times per week.
If you are an athlete, you may not be able to return to full athletic training until 6 months after the surgery. Your doctor of physical therapist will likely advise a gradual return to your previous athletic training or exercising regimen. Back to the surgery list
Rehabilitation after an Arthroscopic Partial Meniscectomy Surgery
A straight forward rehabilitation plan will most likely be given after you have this surgery, as there is little need to protect the tear from further damage because your surgeon has removed it. The surgeon will have removed any displaced or torn tissue in your knee to eliminate your symptoms (popping, locking or clicking of your knee) and improve overall functionality. Early rehabilitation can focus on gaining back range of motion (ROM) as quickly as possible.
Driving after a partial meniscectomy surgery is usually not recommended by doctors until 1 to 2 weeks into rehabilitation. As with any rehabilitation plan, it's important that you consult your doctor, surgeon and/or physical therapist to find out what type of plan will suit your knee and body after your surgery.
Phase 1: Immediate (Acute) Post-Operative Phase
Timeline: surgery completion to 10 days after surgery
The main goals during this Phase of rehabilitation are to reduce inflammation and swelling, restore range of motion and strengthen the quadriceps muscle(s). After a partial meniscectomy surgery improving blood flow function is crucial to reduce the amount of long-term degeneration to your remaining meniscal tissue.
You may wear a brace, but it is generally not required by most doctors or surgeons. You should be able to move around relatively pain free soon after the surgery but may require the use of crutches for your first week of rehabilitation. Your doctor or surgeon will recommend conservative treatments such as R.I.C.E. to reduce pain, inflammation and swelling. Stretching will start early for this surgery - the surgery may even want you to start stretches on the day after your surgery. Stretches will first focus on movement of your quadriceps muscle, hips and gentle extension of your knee. You will also be encouraged to bear as much weight as you possibly can, comfortably, on your affected knee (with the aid of crutches if needed).
As recovery progresses, stretches may increase in number of times and you should be able to gradually stop use of your crutches. You may eventually be limited to using crutches only if absolutely necessary, and limit use to one crutch mid-way through Phase 1 of rehabilitation. Eventually, by the end of this Phase, you will be expected to walk normally (no limping) without the aid of crutches. Limping early on in your rehabilitation is likely to cause compensation pain in your opposite healthy leg, knee, hip and/or back. Limping should be avoided at all costs during rehabilitation.
Your doctor, surgeon or physical therapist will move you onto the next Phase of rehabilitation once you have effectively reduced your pain and swelling with a cold compression, and shown improvement in your range of motion and stretching capability.
Phase 2: Intermediary Post-Operative Phase
Timeline: 10 days to 4 weeks after Surgery
By the end of this Phase in rehabilitation you will be able to have full pain-free range of motion, improved muscle function, and can return to some of your daily activities (work and/or light exercise). Your stretching and strengthening routines will expand to include lunges, squats, full knee extension, hamstring curls, hip movement and balance training. As you progress through this Phase of rehabilitation, your doctor or physical therapist will tweak your stretching and strengthening routine to decrease the number of repetitions for each stretch and instead increase the amount of weight used. Your doctor, surgeon, or physical therapist may integrate a pool program for more intensive running and leg movement, to decrease the amount of weight placed on your knee joints.
Once the surgery skin wound has healed and swelling is down, blood flow enhancer, such as the TShellz Wrap® should be incorporated before exercise to increase localized blood flow in your knee. This will relax muscles and tendons providing enhanced muscular flexibility. You should also continue to use a Cold Compress or Ice Pack to manage pain and swelling occurring after exercise.
Before progressing to the final Phase of rehabilitation for partial meniscectomy surgery, your doctor or physical therapist will expect that you have full pain-free range of motion, absolutely no evidence of swelling or inflammation, and you may be required to pass clinical tests or exams.
Phase 3, Return to Regular Use & Activity
Timeline: 4 weeks after Surgery and Beyond
After 4 weeks of focused rehabilitation for your partial meniscectomy surgery your doctor, surgeon or physical therapist will clear you for a return to all normal activity. You will be need to continue exercise, stretching and strengthening of your knee and surrounding leg muscles in order to maintain full ROM. If you are an athlete, you will likely undergo additional rehabilitation to achieve a gradual return to full athletic activity. Back to the surgery list
When to use a TShellz Wrap (HEAT):
- AFTER the skin wound has fully healed.
- AFTER bruising has significantly reduced.
- NOT WHEN THERE IS SIGNIFICANT SWELLING.
- BEFORE getting out of bed in the morning.
- BEFORE going to bed at night. Never sleep during a treatment.
- BEFORE exercise, workouts or activity of any kind to increase elasticity of joint ligaments & tendons and decrease chance of re-injury.
- Anytime you feel your knee may have stiffened up, is tight and your mobility is reduced causing you more pain.
- Anytime BEFORE you feel you might undertake activity that will put significant strain on the injury area.
- Any other situation where you need to increase blood flow to your knee to relax the joint, relieve trigger point pain / spasms, prevent re-injury and enhance flexibility of soft tissue.
Arnica Pain Cream
Finally, it is worth noting that once you suffer a meniscus tear, you are very likely to notice significant strain happening in your other knee. If this occurs, it is your body telling you that you need to reduce the overall strain on your knees - try to put more of your weight on crutches when you need to walk. Further to this, rest more when possible, use a Cold Compress or Ice Pack when there is swelling and use a TShellz Wrap® when swelling is absent to help keep your "good knee" flexible and prevent further degradation.
Many of our customers have found the Arnica Pain Cream to be quite helpful in keeping pain levels down - both in the torn knee as well as the opposite knee. Just be aware that using a pain cream may reduce the pain but this does not mean your injury is gone.
Learn More About Meniscus Injuries & TreatmentsI want to learn more about Post-Surgery Recovery I want to learn all about Types, Patterns, Shapes & Severity of Meniscus Tears I want to learn more about TShellz Wrap® Circulatory Boost I want to learn more about Ice & Heat: Which Is Better For Treatment? I want to learn more about Meniscus Treatments I want to learn more about different types of Meniscus Surgery FREE SHIPPING ON ALL PRODUCTS CURRENTLY ENABLED
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort at the location of your soft tissue injury until the pain and inflammation settle. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results!
|